Drip And Drive
Have you donated blood lately? Maybe you'll get inspired by reading the history of how we got modern blood donation, including (of course) the bloodmobile.
Today in Tedium: Recently, my wife has really gotten into putting on blood drives, in no small part because of their ability to save lives—by making the iron-laden resources already running through our veins and arteries available to people who need them just a little bit more. These blood drives, quite often, happen in public places. You don’t have to go to the Red Cross; the Red Cross will come to you. Which means that, much like computers, you need to make blood donation stations portable. Possibly on wheels. Today’s Tedium looks into the roots of blood drives and the bloodmobile, which we assume is what the inside of Vampire Weekend’s tour bus must look like. — Ernie @ Tedium
Today’s GIF features a blood bag on a scale. The mechanism is designed to rock the bag gently, so as to mix the blood with anticoagulants (aka blood thinners) and prevent clotting.
[adbox bgcolor=#000000 color=#ffffff accent=#ef2029 background=https://static.tedium.co/2018/03/FP-TediumAd3-FutureCity-800x480.jpg]
What is the one thing designers are tasked with? To imagine the future. Listen to Design Everywhere, the new podcast that invites you to ask ‘what if’ and challenges you to understand ‘the why’ that drives your design. Presented by The Front Porch People, where great conversations happen.
[/adbox]
1628
The year that the circulation of human blood was discovered by English physician William Harvey. Harvey, who spent much of his life trying to understand this process of blood flow, helped create the initial building blocks for blood transfusion. In fact blood transfusions were tried not long after Harvey’s discovery, though it would take nearly 200 years for a human-to-human blood transfusion to be successfully completed—an endeavor pulled off by American physician Philip Syng Physick, who is also nicknamed “the father of American surgery” and is also credited with inventing soda in 1807. (Hopefully he didn’t invent soda and American surgery at the same time.)

(Kzenon/Stockfresh)
Before we had blood banks, we had a cottage industry of on-call blood donors
The problem with blood transfusions, for many years, was preservation.
Once it was clear that blood transfusions between one person and another could be done, this opened up a number of other questions—about compatibility, about safety, about how to maximize this process.
During the late 19th and early 20th centuries, a series of small innovations eventually started to evolve into larger ones. Around this time, understanding into the differences between different types of blood—what would come to be known as Groups A, B, AB, and O, along with a positive or negative designation that refers to the Rh Factor, or the existence of the rhesus protein—was slowly coming into view. The primary blood types were discovered during the first decade of the 20th century; the Rh Factor was a later genetic discovery that effectively doubled the number of total blood types.
But less clear was exactly how a system of blood donations would effectively work. One solution used in the early 1920s involved having an always-at-the-ready bank of volunteers that were ready to share their blood with a patient in need. A 1924 New York Times article highlighted what it called a “new and lucrative trade,” one in which dozens of men were ready to donate their blood at a moment’s notice:
The large New York hospitals have, as a rule, lists of fifty or more men who may be called upon to sell or contribute their blood. These donors, although widely scattered throughout the city, are available at any hour of the day or night, and can be reached usually by telephone. It frequently happens that the life of a patient depends on the operation of a blood transfusion being performed in a few minutes.
An article from the newspaper published during the prior year even nicknamed these blood-donors-by-trade “The Order of Blood Donors.” (I’m assuming this is a turn of phrase, unless this was an actual labor union; of this I can find no evidence beyond the article claiming the donors “have a close knit union.”)
The Times noted that donors, largely men and otherwise manual laborers, were expected to stay in good health and to avoid alcohol, and even after all that, they didn’t even get paid all that much—between $35 to $50 for a case of blood, with perhaps a $5-per-day holding fee around the time that they’re needed. That adds up to around between $500 and $725 today—not exactly a full living wage on its own, and significantly below the average annual income in 1923, which the IRS put at $3,226.70.
“Stories of men who have received fabulous sums for a pint or more of their blood are false and are usually inspired by boasting,” said Thomas Kane, who had undergone an impressive 49 transfusions between 1914 and the time of the 1923 article, or roughly one transfusion every other month.
But this method was clearly inefficient and would not work in every case—say, for example, during wartime, when it would be infeasible to have a bunch of New Yorkers randomly depositing blood at the nearest hospital. While technology was helping to improve matters around the time of World War I—for example, the discovery of blood thinners like sodium citrate—the real breakthrough came just before World War II.
1937
The year that the first blood bank, located in Cook County, Illinois, was created. A concept formulated by a man named Bernard Fantus, a Hungarian doctor who came up with a method of storing blood for up to 10 days. This concept, then one of the medical world’s greatest challenges, was unheard-of at the time, but innovations since have made it possible to store blood for 42 days and blood plasma for as long as a full year in frozen form.
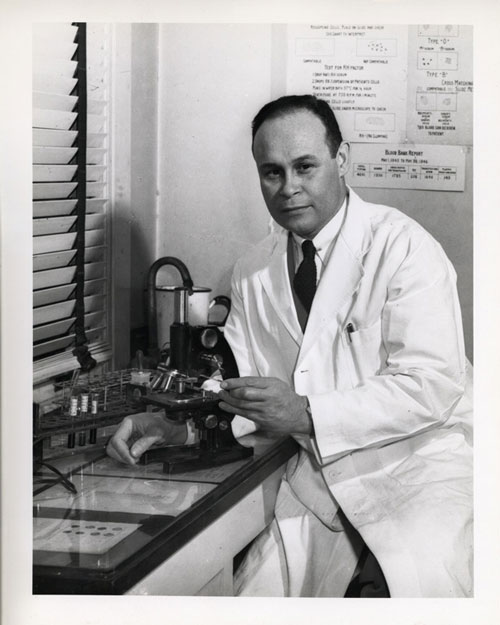
Charles R. Drew. (U.S. National Library of Medicine)
The pivotal figure that set the stage for the modern bloodmobile … and a lot of other things
Broken down, Dr. Charles R. Drew, the first head of the American Red Cross Blood Bank program, worked with the organization for a relatively short period of time, the span of maybe a few months, leaving in favor of a surgical role at Howard University.
And his work was affected by controversy after the fact—as a prominent black doctor, he was critical of the Red Cross for a segregationist policy around blood donations, a move that exposed him to criticism just before the civil rights movement had gained steam.
But what couldn’t be taken away from Drew was that his innovations—including his role in setting the stage for the modern blood bank and the bloodmobile—were both major and tangible works that that save lives up to this day.
That work came to life thanks to the significant amount of research he had done in the years prior. While a doctorate student at Columbia University, Drew spent years analyzing the questions around banking blood, one of the most difficult issues facing the medical industry during the late 1930s and early 1940s. He did so with the support of professor John Scudder, who was also considered an important figure in the mainstreaming of blood donation.
While Drew didn’t invent many of the basic concepts, he did research them at great length, and his doctoral dissertation is an important document that highlights the issues—both medical and practical—that limited the scope of blood donations at that time.
The dissertation, titled “Banked Blood: A Study in Blood Preservation,” discussed different strategies for prolonging the life of blood, with Drew advocating in favor of the use of blood banks in most cases.
“Banked blood is safe when its limitations are known,” he wrote. “The advantage of having ready for instant use bloods of all types is obvious.”
The dissertation and his research into the use of plasma—or the part of blood without any blood cells—earned Drew his doctorate from Columba, making him the first black individual to earn such an honor. His insights into blood and plasma also made him something of a hot commodity in the early days of World War II.
Drew, who had worked on ways to dry plasma for long-term storage while at the university, ended up assisting with the Blood for Britain campaign to send plasma to the United Kingdom. That effort, which the U.S. government viewed as a way to get a grasp a skill that would potentially prove key if the country were brought into the war, was a major success—in no small part thanks to Drew.

A bloodmobile. (Laura Gilmore/Flickr)
After the program ended, Drew was asked to head up the American Red Cross’ first attempts to conduct blood donations on a mass scale. During the months that Drew headed the program, he brought about a number of innovations, including the mobile refrigerated trucks, or “bloodmobiles” to store the blood for later use. The approach solved two problems—it kept the blood usable for longer, and it allowed blood drives to come to where the public was, rather than the other way around.
The Red Cross’ donation program quickly got on the ground running—and starting in 1941, stories highlighting the rise of the bloodmobile started appearing in newspapers all over the country.
At a time when people were looking to assist with the wartime effort at home, donating blood was an excellent way to do just that.
1948
The year that the company Fenwal came up with the plastic blood bag, one of the key pieces of modern blood donation. (The bag design was reportedly quite difficult to get down.) Before the invention of the plastic bag, a glass bottle patented by Drew and Scudder was used instead. The plastic bottle design helped prevent breakage issues that the bottles had.
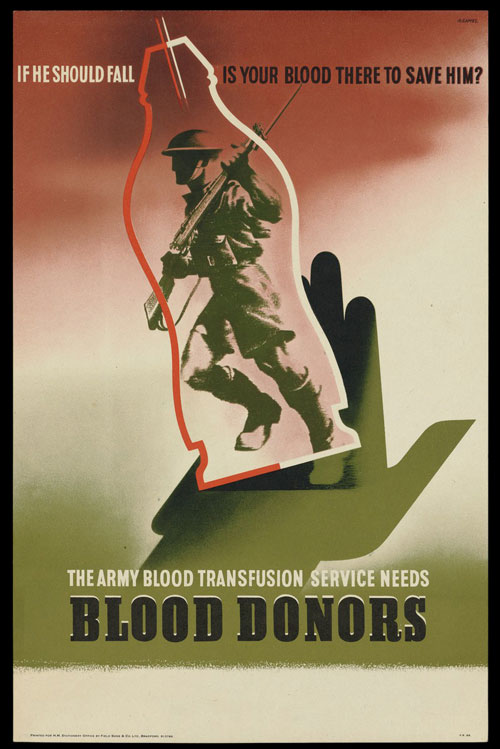
A poster created by the British government to encourage blood donations. (Wellcome Collection)
How segregation complicated the early years of blood donation
The rise of mass-scale blood donation was not without controversy, some of it a result of military pressure on the Red Cross.
The Army and Navy informed the nonprofit they would only accept blood from white donors, and only revised its position the next year to allow donations from other races, but only if the donor types were segregated.
This drew a lot of critics, high among them Drew, who argued that there was no scientific reason for segregating the blood types.
“It was a bad mistake for three reasons: (1) No official department of the Federal Government should willfully humiliate its citizens; (2) There is no scientific basis for the order; (3) They need the blood,” he wrote in a 1944 letter.
He wasn’t alone on that front, but his public criticism of a wartime military decision left him open to critics like Mississippi congressman John Rankin, who preyed on racism in criticizing those who wanted to end the policy.
Drew eventually expanded his criticisms to segregation in the medical field in general—an issue that prevented him and his colleagues at Howard University from becoming, for example, members of the American Medical Association.
In the end, the segregation of blood stuck around throughout the war, but the American Red Cross dropped the policy around 1950. The policy, however, stuck around in some southern states for decades after.
And, of course, it wouldn’t be the only time blood donations ran into social controversy. During the early years of the AIDS crisis, the Food and Drug Administration would bar gay men from donating blood, citing public health concerns; that policy, while softened, still exists in a modified form to this day, and is frequently criticized.
Blood, thanks in no small part to the work of Charles Drew, has become a fundamental tool that saves lives, but it often carries a lot of baggage—cultural baggage.
6.8M
The number of blood donors in the U.S. each year, according to the American Red Cross. Despite that impressive number, the organization notes that the need is never-ending, with around 36,000 units of blood needed every day. The organization says that nearly 40 percent of Americans are eligible to donate blood, but only around 10 percent do so every year.
Charles R. Drew lived an interesting and fundamental life, but in many ways, his story isn’t complete without discussing both his passing and what came after.
In 1950, on his way to a medical conference, he was involved in a serious car accident. He was badly injured, and while attended to quickly by medical officials in North Carolina, he did not survive, dying at the age of 45, but leaving a significant legacy behind—including an entire university named for the man.
Legacy, however, is one of those things that can become complicated in the not-quite-20/20 worldview of history, and at the peak of the civil rights movement, the circumstances around Drew’s story raised a lot of eyebrows after the fact. This had a two-fold effect—it ensured that Drew’s story would not become a footnote, and (more interestingly) it gave his story an element of mythology, where the truth was somewhere in the middle.
The 1996 book One Blood: The Death and Resurrection of Charles R. Drew, written by author Spencie Love, notes how, in the years after his passing, Drew’s life became something of a great myth, with different versions of his story surfacing, often mixing up the details in ways that hurt the public perception of the American Red Cross while making Drew into a sympathetic figure whose life had been damaged by the controversy—or as Love put it, “an increasingly relevant but controversial black folk hero-victim.”
Some versions of the story suggested he quit the Red Cross because of the racism controversy (the U.S. National Library of Medicine, which keeps a digital archive of his writings, says that no evidence exists of this); other versions suggest he was turned away from a whites-only hospital after his car crash because of segregation, and in a dark twist of fate, he bled to death (there is no evidence to suggest this, either, though this urban legend showed up in an episode of M*A*S*H). Other versions still give Drew overwhelming credit in the invention of the technologies we use today in our blood banks and bloodmobiles.
“The legend obviously represents a vast simplification of a very complex historical undertaking that involved many people,” Love wrote. “Drew clearly was not the sole founder of the blood bank or the discoverer of blood plasma, even though he can reasonably lay at least as much claim to these titles as any of the other scientists involved in blood research can.”
When broken down, Drew’s great skill was as an organizer of a very complex system—and at a time when blood donations were evolving away from the idea of on-call donors for hire, that was exactly what was needed. He only spent a few years focused on the issue of blood donations, but he, among others, helped define the way we managed a complex resource—most visibly in the form of those bloodmobiles, where you lay down, drink some juice, and put your blood in a bag for later use.
It’s an important legacy, one you should ponder when you’re noshing on a cookie and waiting around for 15 minutes after you’ve donated your pint.
:format(jpeg)/2018/03/tedium032018.gif)
/2018/03/tedium032018.gif)


/uploads/ernie_crop.jpg)